The Centers for Medicare & Medicaid Services (CMS) Merit-Based Incentive Payment System (MIPS) is the default pathway of the Quality Payment Program (QPP). It requires eligible clinicians to report quality data to earn a performance-based adjustment on their Medicare payments. CMS introduced MIPS in 2017 with an annual ramp-up implementation, meaning each year the requirements change with more points required to avoid penalties, stay neutral or to earn additional payments. There are four components/categories of MIPS:
- Quality component (PQRS)
- Promoting Interoperability (PI) component (formerly Advancing Care Information)
- Improvement Activities (IA) component
- Cost component
Category weights stay the same in 2020
The category weights do not change in 2020 compared to 2019 and remain the same: 45% for quality, 25% for promoting interoperability, 15% for both improvement activities and cost.
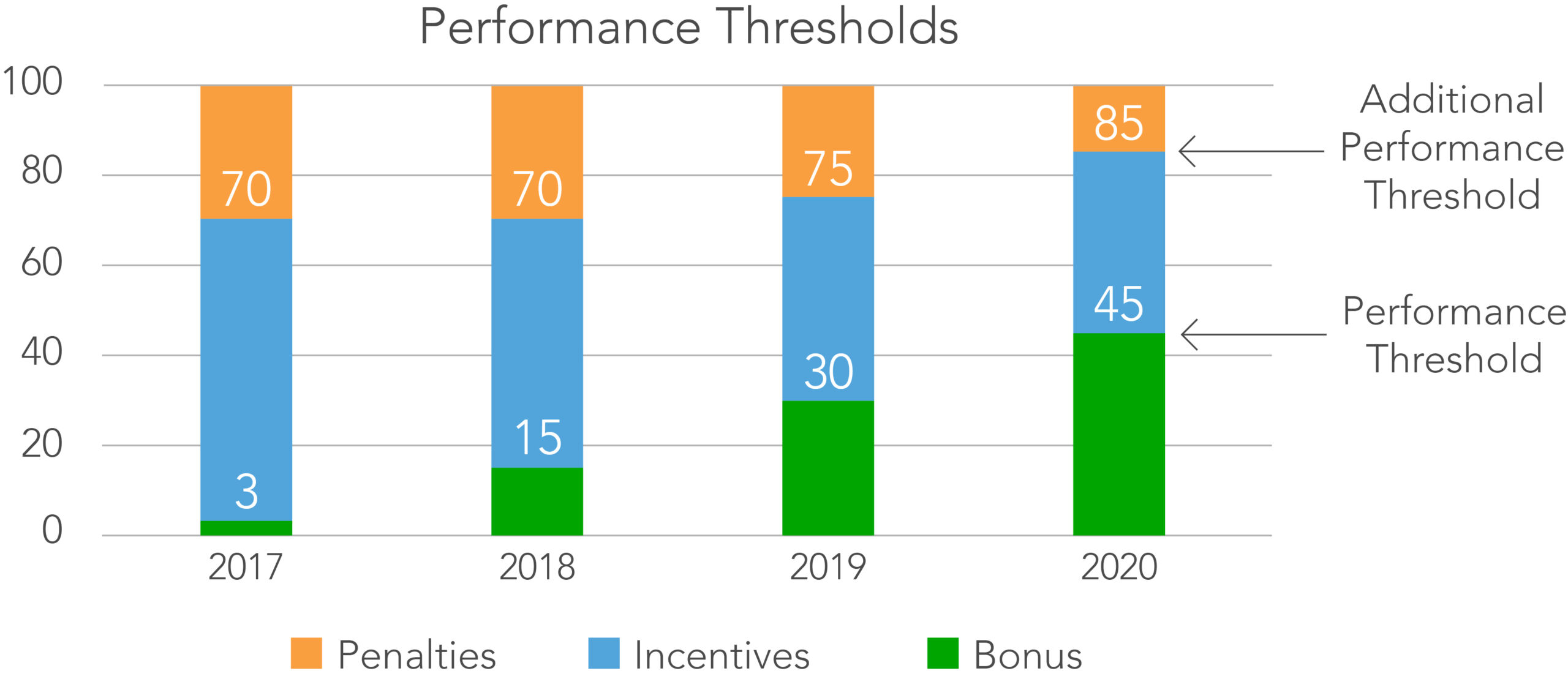
Performance thresholds go up in 2020
In 2020, participating practices will need to find extra 15 points to avoid penalties and 10 points to earn the additional performance bonus. In 2019, practices only needed 30 points to meet the minimum MIPS levels which was raised to 45 for 2020. Equally, those who outperformed in 2019 with MIPS points above 75 points will need 85 points or more to do so in 2020.
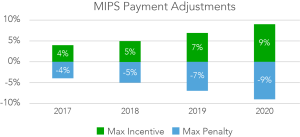
Payment adjustments were raised for 2020
In 2020, the payment adjustment widens to +/- 9%. This is a 2% increase compared to 2019.
Payment adjustments affect groups reporting fewer than 45 points, as it claws back a portion of annual Medicare payments and redistributes it to practices qualifying for additional performance bonus in the form of bonus payments. The CMS estimated the actual positive payment adjustment in 2020 at 6.25%. Given the higher MIPS point requirement for 2020, it is expected more groups will be paying penalties while fewer groups receiving incentives.
Changes in QUALITY category
CMS removed 42 measures for 2020 as certain process measures no longer met the high-priority requirements nor the reporting volumes. This means that, in addition to finding 15 extra points in 2020, some groups might need to seek more due to discontinued measures no longer available in 2020. CMS also increased data completeness to 70% in 2020. That’s 10% more compared to 2019.
CMS added 6 speciality-measure sets for 2020 adding audiology, clinical social work, chiropractic medicine, endocrinology, nutrition/dietician, pulmonology and speech therapy pathology.
Changes in PROMOTING INTEROPERABILITY category
CMS removed the Verify Opioid Treatment measure for 2020. It also now requires 75% of clinicians in a group to be considered hospital-based.
Changes in IMPROVEMENT ACTIVITIES category
CMS increased the participation threshold for groups reporting. Starting 2020, groups earn a credit for an improvement activity if at least 50% of clinicians meet the activity requirement. This is a stark contrast to previous years when only 1 clinician was required to fulfill IA to earn a credit for the group. CMS also made changes to the list by removing, adding and editing some of the improvement activities. In total, 24 changes were made.
Changes in the COST category
CMS revised the Medicare Spending Per Beneficiary measure and the Total Per Capita Cost measure. Additionally, CMS added 10 new measures for 2020.
—
Looking to implement a remote patient monitoring solution? With QardioMD, you can get access to a full remote monitoring end-to-end service to easily track patient data, view patient trends, and make efficient diagnoses. To learn more how RPM with Qardio works, speak with a product expert here.